A 65-year-old patient with a history of chronic anemia is receiving a blood transfusion. Fifteen minutes into the transfusion, the patient reports feeling chills and has a temperature of 101°F (38.3°C). What is the most appropriate initial nursing action?
Stop the transfusion immediately and notify the healthcare provider.
Administer antipyretics and continue the transfusion.
Slow down the rate of the transfusion and reassess in 30 minutes.
Continue the transfusion and monitor the patient closely.
The Correct Answer is A
Choice A Reason:
Stopping the transfusion immediately and notifying the healthcare provider is the most appropriate initial action when a transfusion reaction is suspected. This action helps to prevent further complications and allows for prompt evaluation and management of the reaction. The nurse should also keep the IV line open with normal saline to maintain venous access.
Choice B Reason:
Administering antipyretics and continuing the transfusion is not appropriate. Continuing the transfusion could exacerbate the reaction and lead to more severe complications. The priority is to stop the transfusion and assess the patient before considering any further interventions.
Choice C Reason:
Slowing down the rate of the transfusion and reassessing in 30 minutes is not a safe approach. Any signs of a transfusion reaction, such as chills and fever, require immediate cessation of the transfusion. Delaying intervention could result in worsening of the patient’s condition.
Choice D Reason:
Continuing the transfusion and monitoring the patient closely is not appropriate. Immediate cessation of the transfusion is necessary to prevent further exposure to the potentially harmful blood product. Monitoring alone is insufficient without stopping the transfusion.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["B","C","D","F"]
Explanation
Choice A Reason:
Acetone breath is typically associated with diabetic ketoacidosis (DKA), not hyperosmolar hyperglycemic syndrome (HHS). DKA occurs when there is a significant production of ketones due to the breakdown of fat for energy, leading to a fruity or acetone-like smell on the breath. HHS, on the other hand, does not usually involve significant ketone production.
Choice B Reason:
Fever can be a manifestation of HHS, especially if there is an underlying infection or illness that has precipitated the hyperglycemic crisis. Infections are common triggers for HHS and can contribute to the severity of the condition.
Choice C Reason:
Older age is a risk factor for HHS. HHS is more commonly seen in older adults with type 2 diabetes, often those who have underlying chronic conditions or are experiencing acute illness. The patient’s age of 68 years supports the likelihood of HHS.
Choice D Reason:
A serum glucose level of 800 mg/dL is indicative of HHS. HHS is characterized by extremely high blood glucose levels, often exceeding 600 mg/dL, without significant ketone production. This high glucose level leads to severe dehydration and hyperosmolarity.
Choice E Reason:
A serum bicarbonate level of 15 mEq/L is more indicative of DKA rather than HHS. In HHS, serum bicarbonate levels are typically normal or only mildly decreased because there is no significant ketoacidosis. Therefore, this choice does not support the clinical presentation of HHS.
Choice F Reason:
An insidious onset is characteristic of HHS. Unlike DKA, which can develop rapidly, HHS often develops over days to weeks. Patients may experience gradually worsening symptoms such as increased thirst, frequent urination, and confusion before seeking medical attention.
Correct Answer is A
Explanation
Choice A Reason:
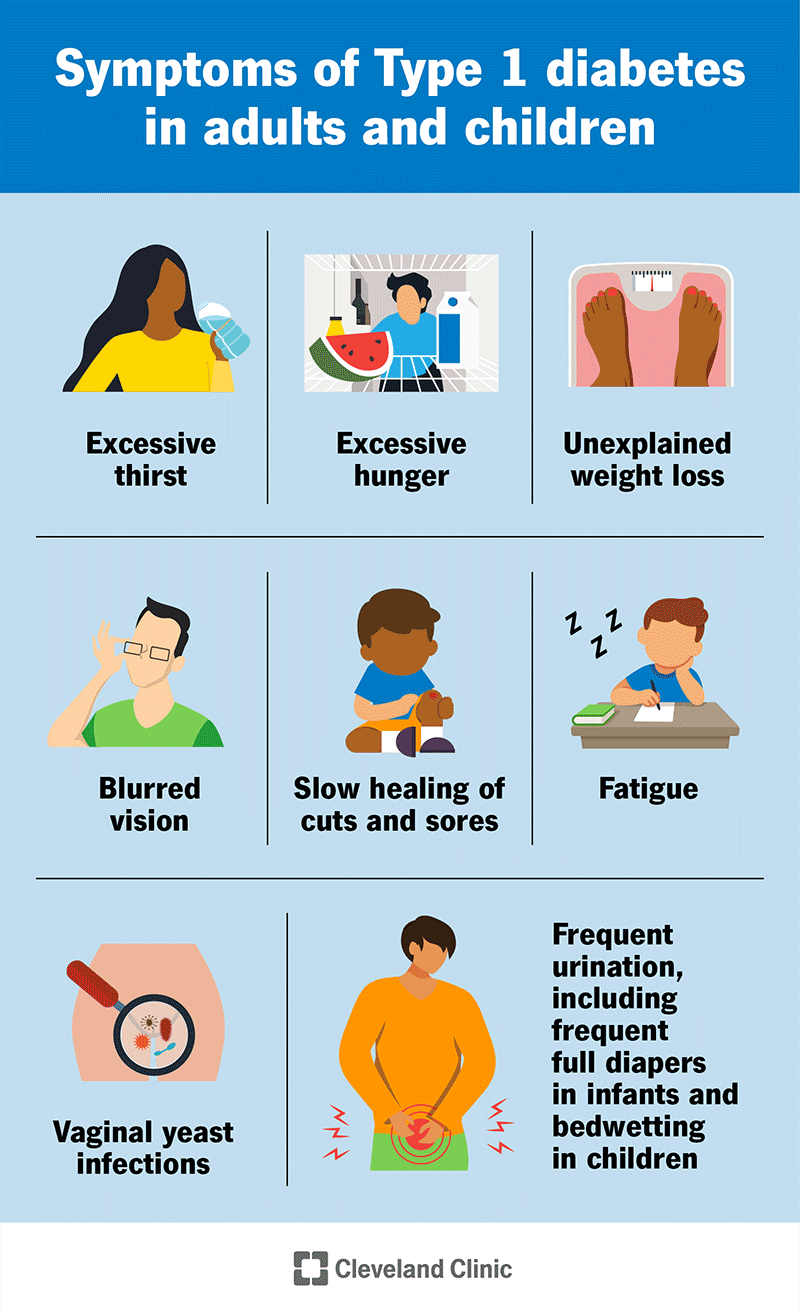
Testing blood glucose levels every 6 hours during illness is crucial for managing type 1 diabetes. Illness can cause blood glucose levels to fluctuate unpredictably, and frequent monitoring helps in making timely adjustments to insulin doses and dietary intake. This practice helps prevent both hyperglycemia and hypoglycemia, ensuring better overall control of diabetes during periods of illness.
Choice B Reason:
Administering the usual daily dose of insulin is important even during illness. Skipping insulin doses can lead to dangerously high blood glucose levels and increase the risk of diabetic ketoacidosis (DKA). It is essential to continue taking insulin as prescribed and to consult with a healthcare provider if any adjustments are needed based on blood glucose readings.
Choice C Reason:
Limiting juices, soda, and gelatin is not typically recommended during illness for patients with type 1 diabetes. These items can be useful for maintaining hydration and providing quick sources of carbohydrates if the patient is unable to eat solid foods. Instead of limiting these items, it is more important to monitor carbohydrate intake and adjust insulin doses accordingly.
Choice D Reason:
Reporting a blood glucose level greater than 300 is critical for preventing complications. High blood glucose levels can indicate the onset of DKA, a serious condition that requires immediate medical attention. Promptly reporting elevated blood glucose levels allows for timely intervention and management to prevent severe complications.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
