Pancreatitis NCLEX questions
The pancreas is a paramount organ in the human body. It’s located behind the lower section of the abdomen near the intestines. The organ produces enzymes that facilitate food digestion and regulate glucose levels in the blood. Pancreatitis NCLEX questions are a big part of the NCLEX for candidates wanting to become registered nurses.
Preparing for the NCLEX test is a challenging undertaking. Adequate time, resources, and effort must be invested in the process. A significant resource that can help you prepare for pancreatitis NCLEX questions is the Naxlex. It’s an award test preparation organization helping thousands of students excel in the NCLEX in the first attempt. Achieve a guaranteed A with Naxlex .
Important content to master in the pancreatitis NCLEX questions
Effective handling of the pancreatitis NCLEX questions demands mastery of the pancreatitis content. Nursing candidates must cover all examinable content before the examination. The following are crucial topics you need to master on the pancreatitis NCLEX items.
-
The fundamentals of pancreatitis
-
Causes and risk factors of pancreatitis
-
Types of pancreatitis (acute and chronic)
-
Pathophysiology of pancreatitis
-
Signs and symptoms of pancreatitis
-
Pathophysiology of pancreatitis
-
Treatment interventions for pancreatitis disorder
The fundamentals of pancreatitis
Pancreatitis is an inflammation of the pancreas that can cause it to be digested by its own enzymes. If it’s not handled effectively, it can cause irreversible damage to the pancreas. The disease can affect people at any age; however, it has been known to affect people aged 30 to 55. The cells in the pancreas perform both exocrine and endocrine functions.
Causes and risk factors of pancreatitis
Risk factors are conditions that increase the chances of suffering from pancreatitis. Several factors can increase a patient’s ability to get pancreatitis. Some of the risk factors include excessive alcohol use, gallstones, certain medications, cystic fibrosis, certain medications, diabetes, abdominal surgery, and smoking. Pancreatitis NCLEX questions contain useful content to prepare for this section of the exam.
Types of pancreatitis (acute and chronic)
There are two known types of pancreatitis: acute and chronic. The name of the pancreatitis can give a hint of the nature of its cause. For instance, acute pancreatitis happens suddenly and can cause organ failure if not handled quickly. Nurses handling the problem need to be well-skilled, which is why the pancreatitis NCLEX questions are such a crucial tool in the study process.
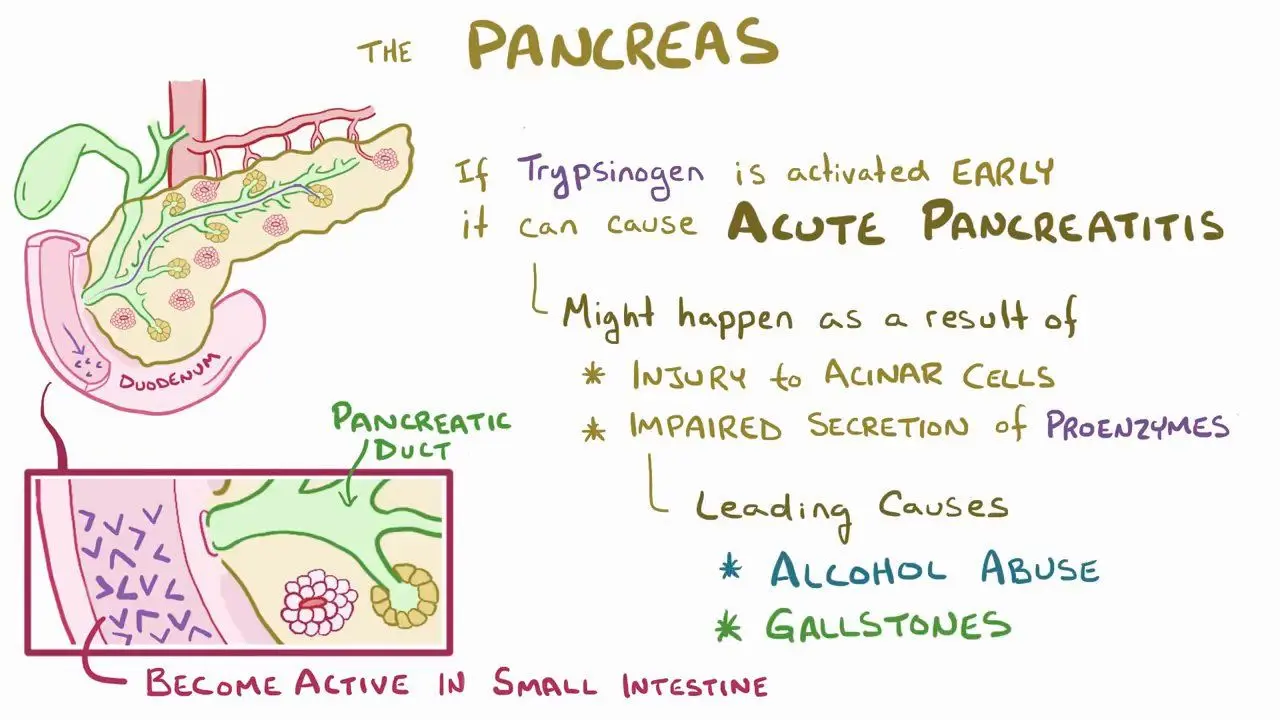
Acute pancreatitis is caused by excessive alcohol use or gallstones. In addition, it can happen following a surgical operation of the gallbladder or pancreas. It manifests as a result of certain treatment drugs such as nonsteroidal anti-inflammatory drugs (NSAIDs) or due to abdominal trauma.
Acute pancreatitis NCLEX questions are popular items in the nursing licensure exam. You can prepare well for acute questions by using the best NCLEX practice questions offered by Naxlex.
Pancreatitis NCLEX questions can give you the skills you need to handle this area well.
Chronic pancreatitis occurs gradually over time. Various known causes of the chronic pancreatitis include diabetes, alcohol abuse, cystic fibrosis, inflammatory bowel disorder, and autoimmune diseases such as lupus erythematosus. The causes of pancreatitis can look broad; however, chronic pancreatitis NCLEX questions can be a good material to help you master the required content.
Pathophysiology of pancreatitis
Understanding the pathophysiology of pancreatitis is crucial to offering tailor-made nursing interventions. The pancreas is an extensive, narrow gland found near the stomach. It helps individuals digest food effectively, produces hormones that regulate blood sugar levels, and produces digestive juices that help break down food.
Pancreatitis occurs when the digestive catalysts are activated while still in the pancreas. This irritates the pancreatitis cells, causing swelling. The inflammation of the pancreas and the presence of active enzymes begin to digest the crucial digestive organ.
Signs and symptoms of pancreatitis
A competent nurse must be able to identify various signs and symptoms of pancreatitis. After assessing the symptoms, the nurse can offer appropriate nursing interventions. Pancreatitis signs vary and include epigastric pain, pain on the left upper quadrant, bruising, jaundice, hypotension, and Turner’s and Cullen’s signs.
Treatment interventions for pancreatitis
Once pancreatitis occurs, effective nursing intervention procedures must be put in place to help the patient recover. Common interventions include assisting in NPO feeding and performing the insertion of a nasogastric tube (NGT) for suctioning. Medication is an important intervention strategy where nurses prescribe appropriate drugs. For example, IV antibiotics are used for pancreatitis treatment. The best IV antibiotics include imipenem 3x500 mg/day i.v. for 14 days.
The nursing interventions to be performed depend on the priorities of the identified problem. For instance, the nursing priority for pancreatitis is to administer intravenous liquids to maintain the client’s hydration balance. Nutritional support is important to ensure the patient is energetic during the treatment process. Conversely, the most important intervention for acute pancreatitis is fluid resuscitation to manage the patient’s condition.
When the prescribed nursing interventions have been done, nurses need to monitor the patient closely. Important signs to monitor include fluid intake and output, diet, pain magnitude, and glucose levels. Monitoring the patient is crucial because any urgent intervention required can be done to save the life of the patient.
Conclusion
The pancreas is a vital organ in the human body. It helps in digestion, produces and regulates blood glucose. Pancreatitis is an inflammation disorder that affects the pancreas. The causes of the disorder include excessive alcohol abuse, smoking, diabetes, cystic fibrosis, and more. The signs and symptoms of the disease include epigastric pain, pain on the left upper quadrant, bruising, jaundice, hypotension, and Turner’s & Cullen’s signs. Once pancreatitis disorder has been identified, nursing interventions include; assistive insertion, medication, and monitoring.
Becoming a licensed nurse requires candidates to pass the NCLEX test. One of the core segments evaluated in the exam is the pancreatitis NCLEX questions. Mastering the entire pancreatitis content requires utilizing good study resources. A great tool that can help you excel in the NCLEX is Naxlex. Our award-winning platform guarantees you an A or 100% money back. Experience the NCLEX difference with Naxlex
Start your journey with us today
Join 1000+ Nursing Students
Powerful learning and clinical tools combined into one platform. The Naxlex Knowledge and Qbanks give you instant and on-the-go nursing knowledge and guidance.