Infection Control
- Infection is the invasion of body tissue by microorganisms with the potential to cause illness or disease1.
- Colonization is the presence of microorganisms on or in a host without causing signs or symptoms of infection2.
- Communicable disease is an infectious disease that can be transmitted from one person to another through direct or indirect contact2.
- Infection control is the practice of preventing and reducing the spread of infections in healthcare settings2.
- Infection control is important for hospitalized children because they are more vulnerable to infections due to their immature immune system, frequent exposure to invasive procedures, and contact with other sick children1.
- The chain of infection is a model that describes how an infection occurs and spreads. It consists of six links: infectious agent, reservoir, portal of exit, mode of transmission, portal of entry, and susceptible host2.
- Infectious agent is a microorganism that causes the infection, such as bacteria, viruses, fungi, or parasites2.
- Reservoir is the place where the infectious agent lives and multiplies, such as humans, animals, soil, water, or medical equipment2.
- Portal of exit is the way the infectious agent leaves the reservoir, such as through respiratory secretions, blood, urine, feces, or wounds2.
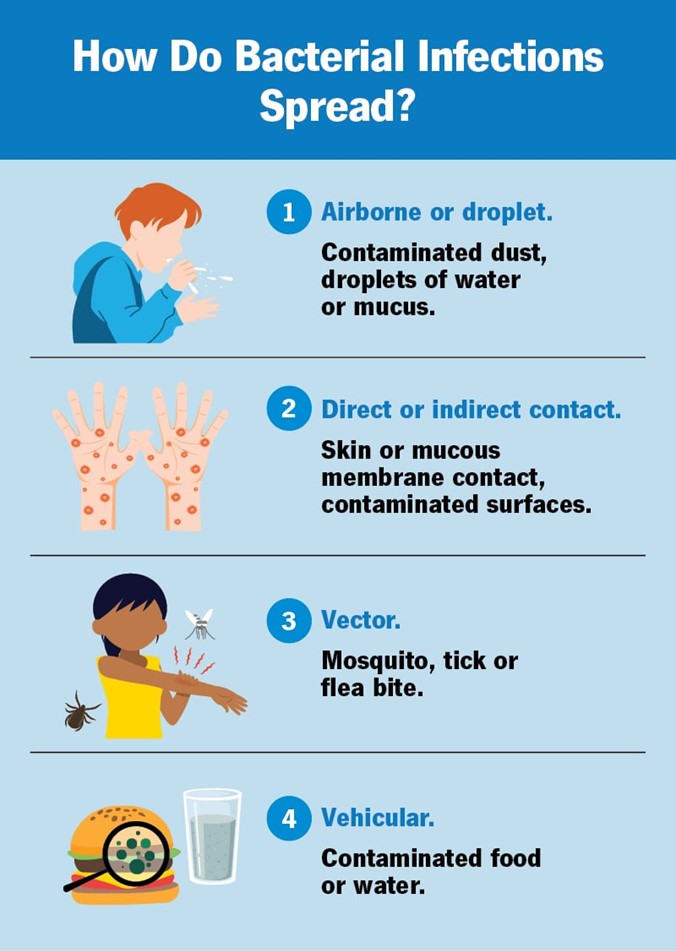
- The mode of transmission is the way the infectious agent travels from the reservoir to the susceptible host. There are four main modes: contact (direct or indirect), droplet, airborne, and vector-borne2.
- Portal of entry is the way the infectious agent enters the susceptible host, such as through mucous membranes, skin breaks, or injection sites2.
- Susceptible host is a person who is at risk of getting infected by the infectious agent. Factors that affect susceptibility include age, immunization status, health condition, and medication use2.
- Hospitalized children are at risk of acquiring two types of infections: healthcare-associated infections (HAIs) and community-acquired infections (CAIs)1.
- HAIs are infections that occur during or after receiving health care services. They are also called nosocomial infections. Examples of HAIs include catheter-associated urinary tract infections (CAUTIs), central line-associated bloodstream infections (CLABSIs), surgical site infections (SSIs), ventilator-associated pneumonia (VAP), and Clostridioides difficile infection (CDI)2.
- CAIs are infections that are acquired outside of healthcare settings. They are also called community-acquired infections. Examples of CAIs include respiratory tract infections (RTIs), gastrointestinal infections (GIs), skin and soft tissue infections (SSTIs), and meningitis1.
- The sources of infection in hospitalized children may vary depending on the type and location of infection. Some common sources are:
- Other infected patients or healthcare workers
- Contaminated medical devices or equipment
- Environmental surfaces or objects
- Visitors or family members
- Animals or insects
- Food or water
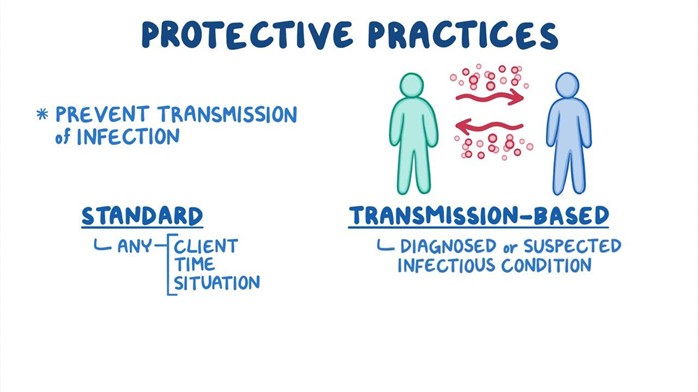
- Standard precautions are the basic level of infection control that should be used for all patients regardless of their diagnosis or presumed infection status. They are based on the principle that all blood, body fluids, secretions, excretions, non-intact skin, and mucous membranes may contain infectious agents2. Standard precautions include:
- Hand hygiene: washing hands with soap and water or using alcohol-based hand rub before and after patient contact, after removing gloves, after contact with potentially infectious materials, and before performing invasive procedures2.
- Personal protective equipment (PPE): wearing gloves, gowns, masks, eye protection, or face shields as appropriate to prevent exposure to blood or body fluids2.
- Respiratory hygiene/cough etiquette: covering mouth and nose when coughing or sneezing, using tissues and disposing them properly, wearing a mask if possible, and maintaining a distance of at least 3 feet from others2.
- Patient placement: assigning patients to private rooms if possible or cohorting them with other patients with the same infection. Isolating patients who pose a risk of transmitting airborne or droplet infections2.
- Environmental cleaning: cleaning and disinfecting frequently touched surfaces and equipment with appropriate agents. Following manufacturer’s instructions for reprocessing reusable medical devices2.
- Waste disposal: disposing of sharps, infectious, and hazardous waste in designated containers. Following local regulations for waste management2.
- Linen handling: handling soiled linen with minimal agitation and wearing gloves and gowns. Placing linen in leak-proof bags and transporting them to laundry facilities2.
- Patient care equipment: using disposable or dedicated equipment for each patient if possible. Cleaning and disinfecting equipment between patient use if shared2.
- Patient education: educating patients and families about the signs and symptoms of infection, the modes of transmission, the prevention measures, and the treatment options1.
- Transmission-based precautions are additional infection control measures that should be used for patients with known or suspected infections that are transmitted by contact, droplet, or airborne routes. They are based on the type of microorganism and the mode of transmission. They are used in addition to standard precautions2. Transmission-based precautions include:
- Contact precautions: used for patients with infections that are spread by direct or indirect contact with the patient or the patient’s environment. Examples of infections that require contact precautions are MRSA, VRE, ESBL, CDI, RSV, scabies, and impetigo2. Contact precautions include:
- Wearing gloves and gowns when entering the patient’s room or having contact with the patient or the patient’s environment2.
- Using disposable or dedicated patient care equipment. Cleaning and disinfecting non-disposable equipment before use on another patient2.
- Placing the patient in a private room or cohorting them with other patients with the same infection. Limiting the movement of the patient outside the room2.
- Educating the patient and family about the infection and the prevention measures1.
- Droplet precautions: used for patients with infections that are spread by large respiratory droplets that are generated by coughing, sneezing, or talking. Examples of infections that require droplet precautions are influenza, pertussis, mumps, rubella, and meningococcal disease2. Droplet precautions include:
- Wearing a mask when entering the patient’s room or having contact with the patient within 3 feet2.
- Wearing eye protection or a face shield if there is a risk of splashes or sprays of respiratory secretions2.
- Placing the patient in a private room or cohorting them with other patients with the same infection. Limiting the movement of the patient outside the room. If the patient needs to be transported, having them wear a mask if possible2.
- Educating the patient and family about the infection and the prevention measures1.
- Airborne precautions: used for patients with infections that are spread by small respiratory droplets that remain suspended in the air and can be inhaled by others. Examples of infections that require airborne precautions are tuberculosis, measles, chickenpox, and disseminated herpes zoster2. Airborne precautions include:
- Wearing a respirator (such as N95) when entering the patient’s room or having contact with the patient2.
- Placing the patient in a private room with negative air pressure and 6 to 12 air changes per hour. Keeping the door closed at all times. Limiting the movement of the patient outside the room. If the patient needs to be transported, having them wear a mask if possible2.
- Educating the patient and family about the infection and the prevention measures1.
- Contact precautions: used for patients with infections that are spread by direct or indirect contact with the patient or the patient’s environment. Examples of infections that require contact precautions are MRSA, VRE, ESBL, CDI, RSV, scabies, and impetigo2. Contact precautions include:
Chain of infection and modes of transmission
Risk factors and sources of infection in hospitalized children
Standard and transmission-based precautions
Nursing Test Bank
Quiz #1: RN Exams Pharmacology Exams
Quiz #2: RN Exams Medical-Surgical Exams
Quiz #3: RN Exams Fundamentals Exams
Quiz #4: RN Exams Maternal-Newborn Exams
Quiz #5: RN Exams Anatomy and Physiology Exams
Quiz #6: RN Exams Obstetrics and Pediatrics Exams
Quiz #7: RN Exams Fluid and Electrolytes Exams
Quiz #8: RN Exams Community Health Exams
Quiz #9: RN Exams Promoting Health across the lifespan Exams
Quiz #10: RN Exams Multidimensional care Exams
Naxlex Comprehensive Predictor Exams
Quiz #1: Naxlex RN Comprehensive online practice 2019 B with NGN
Quiz #2: Naxlex RN Comprehensive Predictor 2023
Quiz #3: Naxlex RN Comprehensive Predictor 2023 Exit Exam A
Quiz #4: Naxlex HESI Exit LPN Exam
Quiz #5: Naxlex PN Comprehensive Predictor PN 2020
Quiz #6: Naxlex VATI PN Comprehensive Predictor 2020
Quiz #8: Naxlex PN Comprehensive Predictor 2023 - Exam 1
Quiz #10: Naxlex HESI PN Exit exam
Quiz #11: Naxlex HESI PN EXIT Exam 2
Questions on Infection Control
Correct Answer is A
Explanation
<p>Choice D reason: This is not the correct answer, as the mode of transmission is the fourth link in the chain of infection. It is the way that the infectious agent travels from one host to another, such as through direct or indirect contact, droplet, airborne, vector, or vehicle transmission.</p>
Correct Answer is ["A","B","C","D"]
Explanation
This factor may not have contributed to the development of an HAI, as CAIs are infections that are acquired outside of health care settings. However, CAIs may increase the risk of HAIs if they are not treated properly or if they cause complications.
Correct Answer is A
Explanation
This statement by the nurse would not be appropriate to educate the child and family about chickenpox, as it incorrectly describes the infectious agent and mode of transmission for this condition. Chickenpox is not caused by a parasite or spread through bites from mosquitoes or ticks.
Correct Answer is A
Explanation
<p>Choice D reason: This is not the correct answer, as droplet precautions are additional infection control practices that should be used for patients who have infections that can be spread by large droplets that are generated by coughing, sneezing, or talking and can be transmitted to others who are within 3 feet of the patient. They include wearing a surgical mask, placing the patient in a private room or cohorting with other patients with the same infection, and limiting patient movement outside the room. A positive pressure room may also increase the risk of spreading the infection to other areas of the hospital.</p>
Correct Answer is D
Explanation
This statement by the nurse would be most appropriate to include in the teaching, as it helps prevent the occurrence and spread of common infectious diseases that can cause serious complications or death. Vaccination is one of the most effective ways to protect oneself and others from CAIs.
Questions on Standard and transmission-based precautions
Correct Answer is A
Explanation
<p>Choice D reason: This is not the correct answer, as gloves are not sufficient PPE to wear when performing urinary catheter care for a patient who has a UTI. Gloves protect the nurse's hands from exposure to urine, but they do not protect the nurse's clothing and skin from contamination by urine or other body fluids.</p>
Correct Answer is ["A","B","C","E"]
Explanation
This action should be taken as part of standard precautions, as it helps prevent the transmission of microorganisms through environmental surfaces or objects.
This statement by the nurse would not be appropriate to educate the patient and family about TB, as it incorrectly describes the infectious agent and mode of transmission for this condition. TB is not caused by a parasite or spread through ingestion of contaminated food or water.
<p>Choice D reason: This is the correct answer, as gloves and respirator are the appropriate PPE to wear when entering the room of a patient who has measles. Gloves protect the nurse's hands from exposure to blood or body fluids, and the respirator protects the nurse's respiratory tract from
<p>Choice D reason: This is not the correct answer, as neutropenic precautions are indicated for patients who have low white blood cell counts and are at risk of developing infections from normal flora or environmental sources. CDI is not caused by normal flora or environmental sources, but by an ov
<p>reason: This is the correct answer, as all of the above actions should be taken by the nurse to prevent cross-contamination. MRSA is a serious and potentially life-threatening infection that can cause skin and soft tissue infections, bloodstream infections, pneumonia, or surgical site infections.
<p>Choice D reason: This is not the correct answer, as neutropenic precautions are indicated for patients who have low white blood cell counts and are at risk of developing infections from normal flora or environmental sources. Influenza is not caused by normal flora or environmental sources, but by
This statement by the nurse would be appropriate to include in the teaching, as it helps reduce the exposure of the patient to potential sources of infection from visitors and protect them from transmitting any infection to others.
Questions on Safety measures
Search Here
Related Topics
- Stages of physical, cognitive, social and emotional development from infancy to adolescence - Nursing Care of Hospitalized Children
- Developmental milestones and screening tools - Nursing Care of Hospitalized Children
- Factors affecting growth and development - Nursing Care of Hospitalized Children
- Interventions to promote optimal development - Nursing Care of Hospitalized Children
- Conclusion - Nursing Care of Hospitalized Children
More on Nursing
Free Nursing Study Materials
Access to all study guides and practice questions for nursing for free.
- Free Nursing Study Trials
- Free Nursing Video tutorials
- Free Nursing Practice Tests
- Free Exam and Study Modes
- Free Nursing Revision Quizlets
