The ED nurse is caring for a client who has gone into cardiac arrest.
During external defibrillation, what action should the nurse perform?
Continue to ventilate the client via endotracheal tube during the procedure
Ensure no one is touching the client at the time shock is delivered
Allow at least 3 minutes between shocks
Place gel pads over the apex and posterior chest for better conduction
The Correct Answer is B
Choice B rationale:
It is crucial to ensure that no one is touching the client during defibrillation to prevent accidental electrical shock to others. The electrical current delivered by the defibrillator is extremely powerful and can cause serious injury or even death if it passes through another person's body. This includes both healthcare professionals and bystanders.
Here are key points to emphasize this rationale:
Electrical conduction: The human body is a good conductor of electricity. If someone is touching the client during defibrillation, the electrical current from the defibrillator can easily pass through their body, potentially causing harm.
Cardiac rhythm disruption: Any contact with the client during shock delivery can interfere with the defibrillator's ability to accurately assess the client's heart rhythm and deliver the appropriate shock. This could potentially worsen the client's condition.
Muscle contractions: The electrical current from the defibrillator can cause involuntary muscle contractions. If someone is touching the client, these contractions could cause them to jerk or move suddenly, potentially causing injury to themselves or others.
Safety guidelines: It is a standard safety guideline in all healthcare settings to clear the area around a client before defibrillation to ensure the safety of everyone involved.
I'll now address the other choices, even though they are not the correct answer, to provide a comprehensive understanding:
Choice A rationale:
While ventilation is important during cardiac arrest, it should be temporarily paused during defibrillation. The chest compressions and electrical shock can cause movement of air in the lungs, which can interfere with the effectiveness of the defibrillation. Additionally, the risk of accidental shock to the person providing ventilation is increased if they are close to the client during defibrillation.
Choice C rationale:
Waiting 3 minutes between shocks is not necessary with modern defibrillators. Current guidelines recommend immediate defibrillation for shockable rhythms such as ventricular fibrillation or pulseless ventricular tachycardia. Delaying defibrillation can decrease the chances of successful resuscitation.
Choice D rationale:
The placement of gel pads is important for effective conduction, but it is not the priority action during defibrillation. Ensuring safety by clearing the area and delivering the shock promptly is more critical in the initial moments of defibrillation.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A rationale:
Antipyretic action refers to the ability to reduce fever. While aspirin does have antipyretic properties, this is not the primary reason it is administered during an MI. Fever is not a characteristic symptom of MI, and reducing fever would not directly address the underlying cause of the MI, which is the formation of a blood clot in a coronary artery.
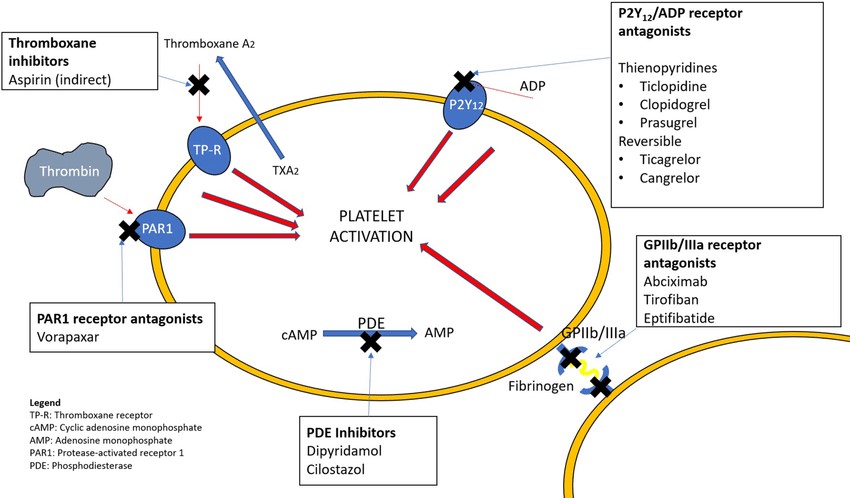
Choice B rationale:
Antiplatelet action is the ability to prevent platelets from clumping together and forming blood clots. This is the crucial mechanism by which aspirin helps in the setting of an MI.
During an MI, a blood clot forms in a coronary artery, blocking blood flow to the heart muscle. This blockage can cause severe damage to the heart muscle, leading to chest pain, shortness of breath, and potentially life-threatening complications.
Aspirin irreversibly inhibits the enzyme cyclooxygenase (COX), which is essential for platelet aggregation. By blocking COX, aspirin prevents platelets from sticking together and forming new clots. This can help to:
Limit the size of the existing clot in the coronary artery.
Prevent the formation of additional clots that could further block blood flow.
Allow for better blood flow to the heart muscle, reducing damage and improving outcomes.
Choice C rationale:
Analgesic action refers to the ability to relieve pain. While aspirin does have analgesic properties, this is not the primary reason it is administered during an MI. Pain relief is an important aspect of managing MI symptoms, but it does not directly address the underlying cause of the MI, which is the blood clot.
Choice D rationale:
Antithrombotic action is a broader term that encompasses any action that prevents or reduces blood clot formation. Aspirin's antiplatelet action is a specific type of antithrombotic action. However, it's important to note that aspirin does not directly dissolve existing clots; it primarily prevents new clots from forming.
Correct Answer is ["A","C","D"]
Explanation
Choice A rationale:
Duration of pain: Stable angina typically lasts for less than 5 minutes, while pain from a myocardial infarction (MI) typically lasts longer, often 20 minutes or more. This is because stable angina is caused by a temporary decrease in blood flow to the heart muscle, while an MI is caused by a complete blockage of blood flow, leading to more severe and prolonged pain.
Mechanism of pain: The pain in stable angina is due to ischemia, which is a lack of oxygen to the heart muscle. This occurs when the demand for oxygen by the heart muscle exceeds the supply of oxygenated blood.
Nitrates and ischemia: Nitrates, such as nitroglycerin, work by dilating the coronary arteries, which increases blood flow to the heart muscle and relieves ischemia. This is why nitroglycerin is often effective in relieving the pain of stable angina.
Choice B rationale:
Non-specific symptom: Shortness of breath can occur with both stable angina and MI, as well as other conditions such as lung disease or anxiety. Therefore, it is not a specific symptom that can be used to differentiate between the two conditions.
Choice C rationale:
Activity level: Stable angina is typically triggered by exertion or emotional stress, which increase the heart's demand for oxygen.
Rest and angina: The pain often subsides with rest or nitroglycerin.
MI and rest: In contrast, the pain of an MI can occur at rest and is not always relieved by nitroglycerin.
Choice D rationale:
Nitrates and stable angina: As mentioned earlier, nitrates are often effective in relieving the pain of stable angina.
Nitrates and MI: However, they may not be as effective in relieving the pain of an MI, as the blockage of blood flow is more severe.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
